Your condition involves narrowing of the cervical spinal canal discovered on imaging that appears to have no current symptoms nor findings on exam and therefore surgery is not indicated at this point even though there is pressure to some degree on your spinal cord. Neck pain without other red flag symptoms does not warrant surgical recommendations.
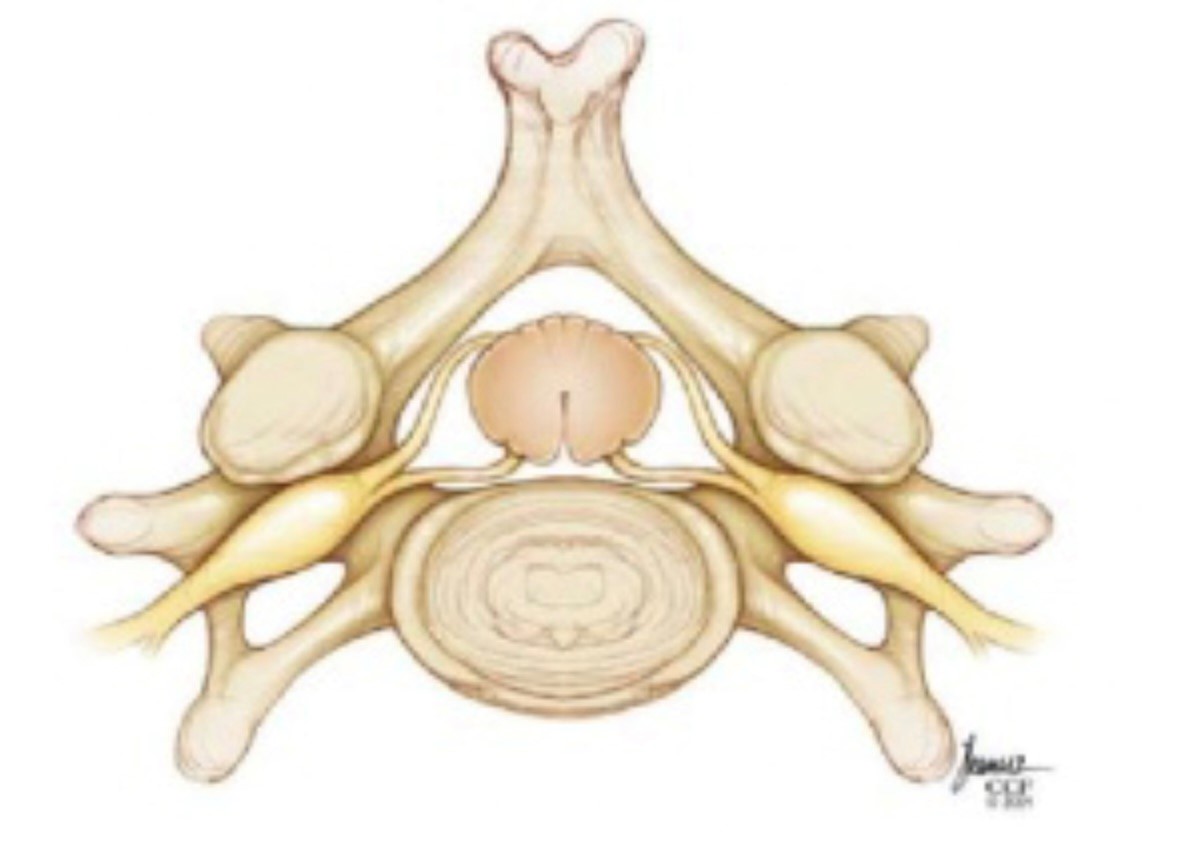
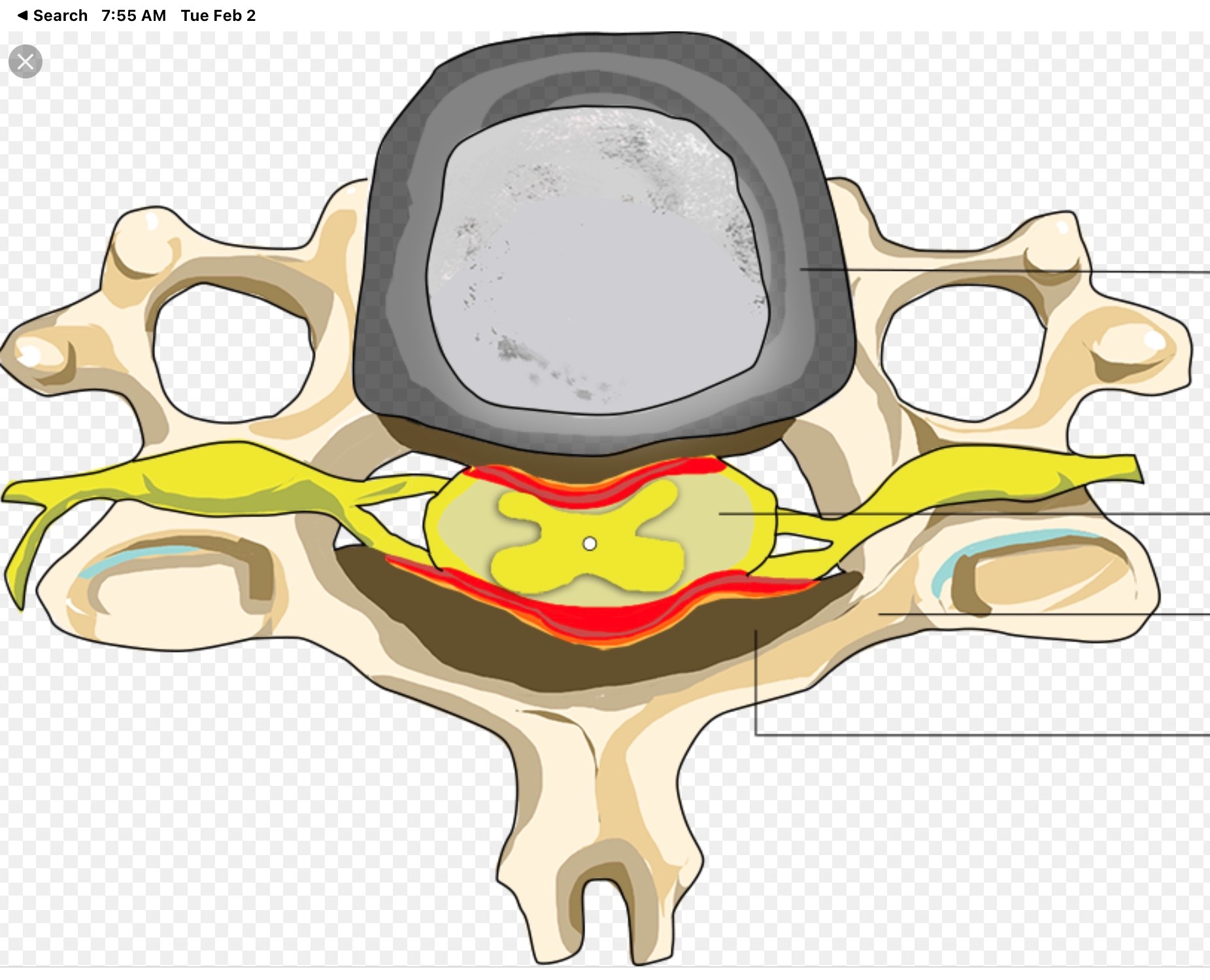
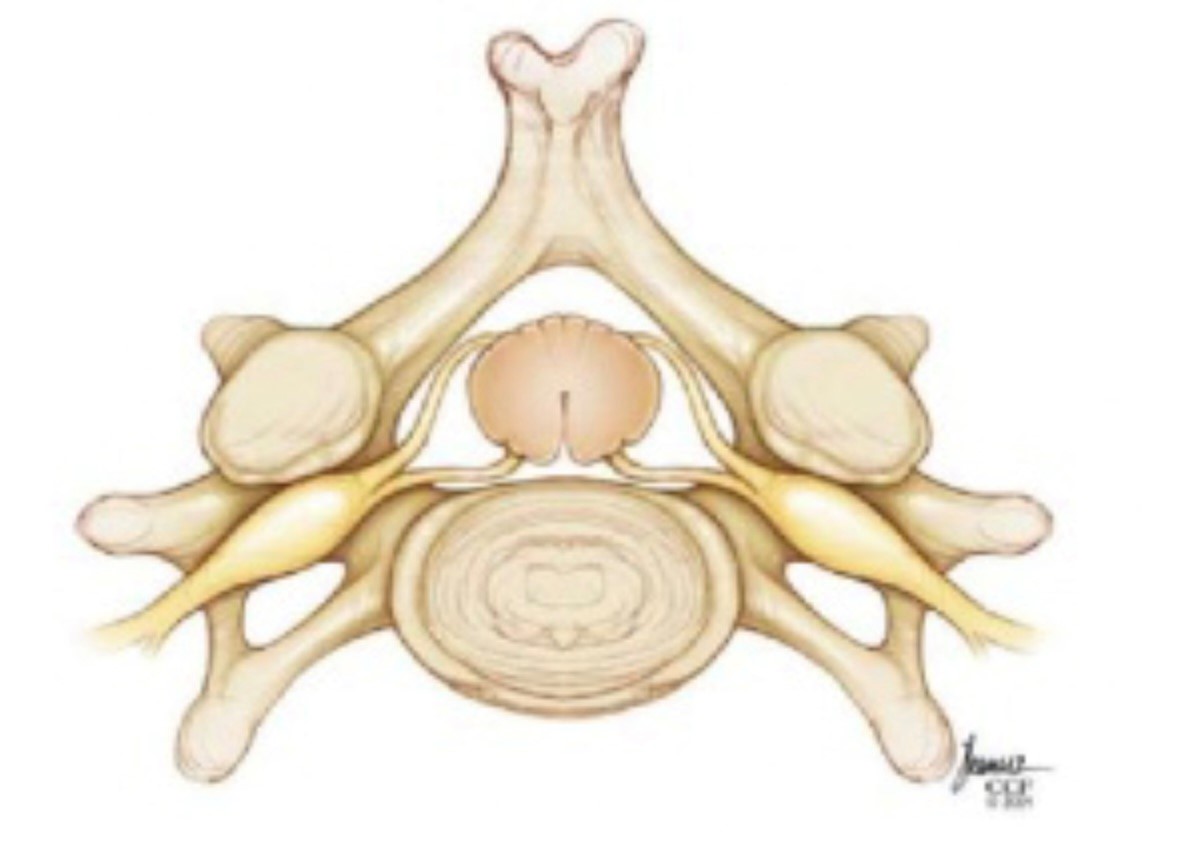
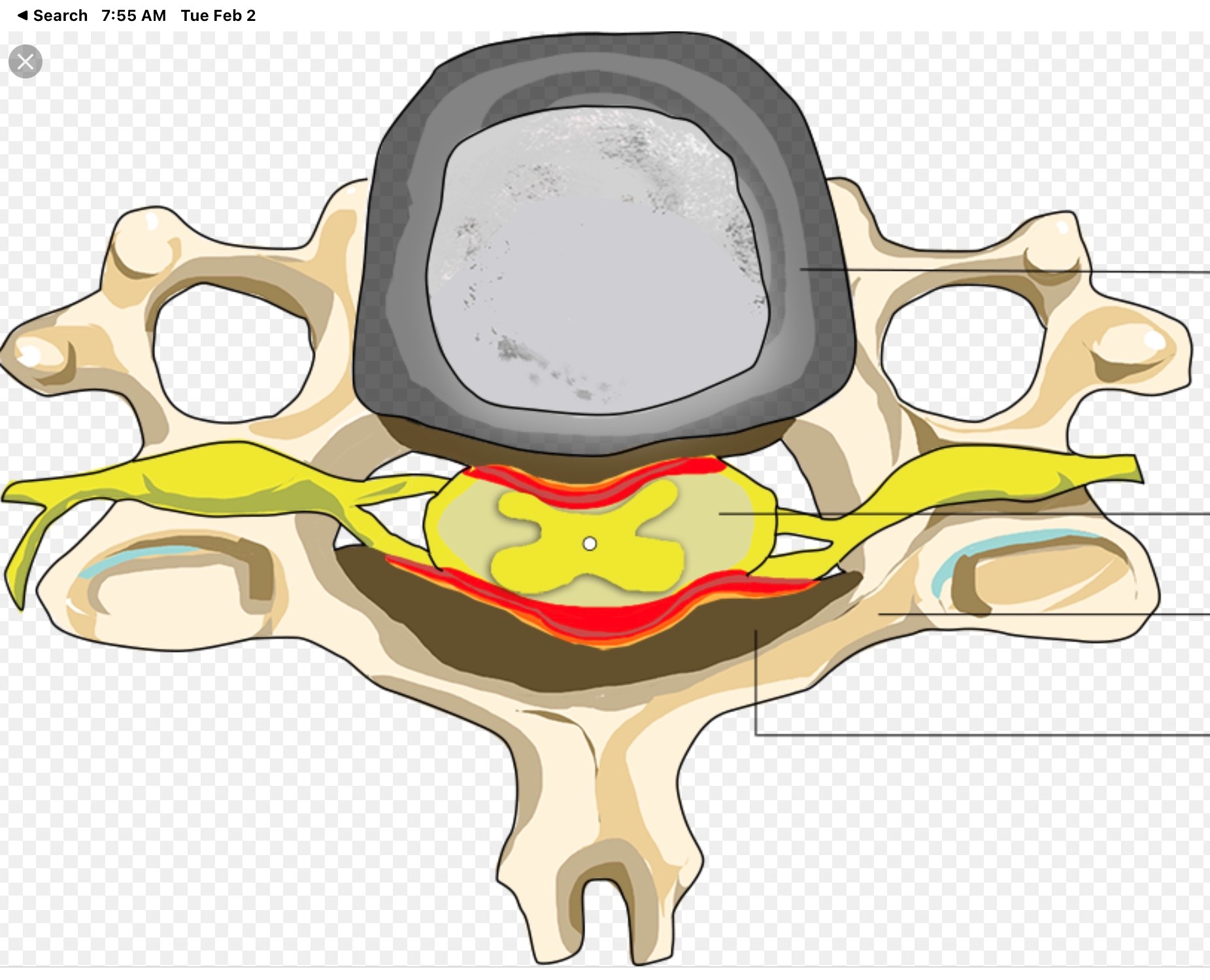
Normal Canal Cervical Stenosis
Why one person with cervical spinal stenosis is having major symptoms and another with the same MRI findings has none is unknown but very commonly seen.
In the normal spinal canal the spinal cord floats freely in the cerebrospinal fluid, CSF or spinal fluid, which serves as a protective shock absorber. In patients with Cervical Spinal Stenosis the amount of CSF around the spinal cord is markedly diminished reducing the ability to protect the spinal cord from normal impacts or stronger forces. This increases the risk of injury to the spinal cord from various normally tolerated forces. You have seen this in football games when a player gets a sudden hard impact to the head and neck and suddenly goes paralyzed. Most of these patients had this impact injury develop due to having such a blow in the setting of previously asymptomatic cervical spinal stenosis that was likely present since birth but never known to exist until the injury. Fortunately the NCAA and NFL have focused on these “targeting” incidents in recent years.
Most of the time if the patient has no symptoms neurosurgeons will suggest non surgical follow up observation only with recommendations to avoid high risk activities unless:
- The cervical spinal stenosis is particularly severe in degree
- There is associated with spinal cord edema
- The patient’s career has unavoidable risk of high impact injuries
- The patient has no symptoms yet does have positive findings on neurological examination of spinal cord dysfunction
- The cervical spinal stenosis is progressively worsening on follow up MRI scans
Many patients ask why do we not go ahead and do surgery if there is cervical spinal stenosis even without symptoms or exam findings?
The answer:
- The risk of surgery for cervical spinal stenosis must be weighed against the risk of observation. In most patients who are without symptoms the risk benefit ratio favors observation only.
- Most people who have asymptomatic cervical spinal stenosis do not ever develop the need for surgery by never becoming symptomatic nor showing exam findings of spinal cord dysfunction nor significant MRI worsening during follow up over time.
- Most asymptomatic patients that ultimately become symptomatic and need surgery for cervical spinal stenosis will develop warning or red flag minor symptoms early enough that they usually have no long term side effects from not having surgery done prior to symptoms.
- Most patients with asymptomatic cervical spinal stenosis do not suddenly go paralyzed from their condition, unless there is a major impact injury that would likely injure even a patient without cervical spinal stenosis, but rather develop slowly progressive red flag symptoms
- Medical studies on asymptomatic cervical spinal stenosis consistently support the role of observation vs prophylactic surgery.
When non-surgical observation only is the plan it is recommended that you avoid:
- Sports and non sports axial load injuries
- High-energy impact sports such as skydiving, downhill skiing, cliff climbing, football etc
- Falls
- Car, bike and motorcycle accidents whenever possible
- Forceful Manipulation of the head and neck including physical therapist or chiropractic neck manipulation
The above is recommended in order to mitigate the increased risk of spinal cord injury in patients with cervical stenosis as compared to someone with a normal spinal canal. Again people without cervical spinal stenosis have risks of spinal cord injury and paralysis with the above but those with cervical spinal stenosis have a statically increased risk of injury with the same force applied as compared to a person with a normal spinal canal. Nevertheless, the same applies to breaking a leg or an arm from a fall in patients with osteoporosis versus normal bone. We would not recommend putting casts on all the limbs of osteoporotic patients to prevent fractures from a fall!
Typically if non surgical treatment is the plan you will be followed up after a period of time with a clinical follow up visit +/- a follow up MRI at variable intervals for years to come and be advised to contact your neurosurgeon sooner if you develop any concerning red flag symptoms listed below.


Once patients develop symptoms and/or findings on exam then the condition is called “cervical myelopathy”. Typically the MRI will show abnormal signal changes like the images above due to edema of the spinal cord in patients that are symptomatic from the cervical spinal stenosis. This term is used to describe dysfunction of the spinal cord from many causes but in this case it is due to cervical spinal stenosis and the damage from the pressure on the actual spinal cord.
MANY PATIENTS WITH SYMPTOMATIC CERVICAL SPINAL STENOSIS, MYELOPATHY, WILL HAVE LITTLE TO NO NECK OR ARM PAIN BUT RATHER ONE OR MORE OF THE NON PAINFUL RED FLAGS BELOW.
Red flag symptoms to be aware of that might be indicative of cervical stenosis becoming symptomatic include any of the following:
- Development of numbness and tingling in the arms and/or hands
- Development of electric shock sensations that run down the spine or through the extremities with such activities as movement of the neck or coughing, sneezing or bowel movements etc. (Lhermitte’s phenomenon)
- Development of pain running from the neck down one arm of the other or both.
- Development of clumsiness or loss of dexterity with loss of fine motor movement of the fingers and of the hands. This may evidenced as problems buttoning ones shirt or developing problems writing with a pen or clumsiness typing with a keyboard.
- Development of unsteadiness and clumsiness of gait while walking. This may present as stumbling when walking for no apparent reason. This is particularly noticeable when present during attempts to perform field sobriety testing, tandem gait testing or walking placing one foot immediately in front of the other while trying to walk a straight line
- Development of significant weakness of the arms and hands that may present with inability and to normally use one’s hands and arms in the normal course of work and or play activities
- Development of clumsiness and dysfunction and stiffness of the muscles of the upper or lower extremities (spasticity)
- Development of urinary &/or bowel incontinence particularly associated with symptoms above is a typically a very late symptom. Isolated urinary problems would be uncommon due to cervical spinal stenosis and more likely related to urological/GI disorders.
If symptoms develop or MRI findings worsen or findings on neurological exam appear then surgery will likely be needed.
When needed surgery can be either an anterior cervical decompression and fusion surgery or a posterior cervical decompression with or without fusion or both depending on your anatomy.
Hopefully your cervical spinal stenosis will never need treatment but please carefully read the warnings above and be mindful of the red flag symptoms discussed. Please report to your neurosurgeon development of any concerning symptoms when they develop. Do not wait for the follow up visit if these symptoms develop sooner. Regardless, keep your scheduled follow up plan even if you have zero symptoms and are pain free!
Any questions or concerns visit legacyneuro.com
Scott Schlesinger MD
Legacy Spine and Neurological Specialists
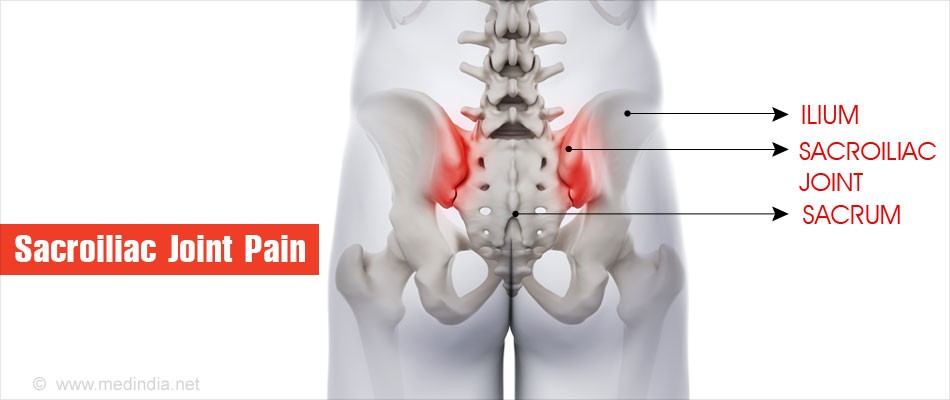 when the body bears weight or flexes forward. Arthritic and certain age-related degenerative disorders may gradually erode protective joint cartilage, which can subsequently lead to instability and pain that can mimic some of the symptoms of lumbar pathologies.
when the body bears weight or flexes forward. Arthritic and certain age-related degenerative disorders may gradually erode protective joint cartilage, which can subsequently lead to instability and pain that can mimic some of the symptoms of lumbar pathologies.