Do you have SI Joint Pain?
The SI joint can be a significant cause of lower back pain. Clinical publications have identified the SI joint as a pain generator in 15-30% of chronic lower back pain patients.1-4 In addition, the SI joint is a pain generator in up to 43% of patients with continued or new onset lower back pain after a lumbar fusion.5
Sacroiliac Joint (SI Joint) Anatomy
The sacroiliac joint (SI joint) is located in the pelvis; it links the iliac bones (pelvis) to the sacrum (lowest part of the spine above the tailbone). It is an essential component for energy transfer between the legs and the torso.
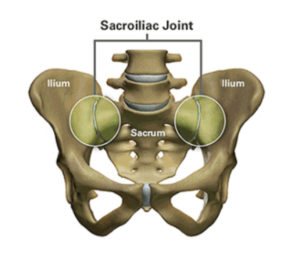
The SI-joint is the link between the ilium in the pelvis to the sacrum, which is the lowest part of the spine above the tailbone.
Like any other joint in the body, the SI joint can be injured and/or undergo degeneration. When this happens, people can feel pain in their buttock and sometimes in the lower back, hips and legs. This is especially true while lifting, running, walking or even lying on the involved side.

Excessive motion in the SI joint may inflame and disrupt the joint and surrounding nerves causing pain in the lower back, hip, groin, or pelvis.
It’s common for pain from the SI joint to feel like disc or lower back pain, or sometimes hip or groin pain. For this reason, SI joint disorders should always be considered in lower back, hip, and pelvic pain diagnosis.
Do you experience one or more of the symptoms listed below?
- Lower back pain
- Sensation of low extremity: pain, numbness, tingling, weakness
- Pelvis/buttock pain
- Hip/groin pain
- Feeling of leg instability (buckling, giving way)
- Disturbed sleep patterns due to pain
- Disturbed sitting patterns (unable to sit for long periods, sitting on one side)
- Pain going from sitting to standing
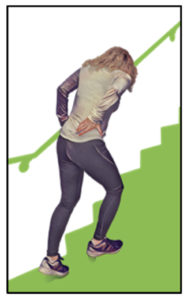
PAIN STEPPING UP:
PAIN ON TRANSITIONAL MOVEMENTS:
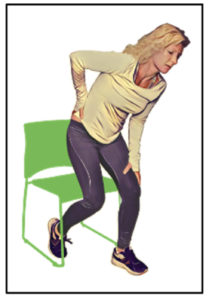
Patients who suffer from Sl joint dysfunction can have severe pain when performing transitional movements like standing from a chair.
PAINFUL SITTING:

Patients who have SI joint pain usually find it difficult to sit for long periods of time, and usually try to alleviate the discomfort by sitting on the least effected side.
Making a Diagnosis
A variety of tests performed during physical examination may help reveal the SI joint as the cause of your symptoms. Sometimes, X-rays, CT-scan or MRI may be helpful in the diagnosis of SI joint-related problems because they can rule out other common sources of pain—such as your lumbar spine or hip joints. It is also important to remember that other conditions (like a disc problem) can co-exist with SI joint disorders.
The most relied upon method to accurately determine whether the SI joint is the cause of your lower back pain symptoms is to inject the SI joint with a local anesthetic. This diagnostic injection will be performed under either X-ray or CT guidance to verify accurate placement of the needle in the SI joint. If your symptoms decrease by at least 50%, it can be concluded that the SI joint is either the source of or a major contributor to your lower back, hip, or pelvic pain. If the level of pain does not change after SI joint injection, it is less likely that the SI joint is the cause of your pain.
Treatment Options
Once the SI joint is confirmed as the cause of your symptoms, treatment can begin. Some patients respond well to physical therapy, use of oral medications, or injection therapy. These treatments are often performed repetitively, and frequently symptom improvement using these therapies is temporary. If non-surgical treatment options have been tried and do not provide long-term relief, your surgeon may consider other options, including the minimally invasive iFuse procedure.
SI Joint Fusion with the iFuse Implant System®
Dr. Dominic Maggio is trained in the latest minimally invasive surgical (MIS) techniques, including use of the iFuse Implant System® from SI-BONE®, a medical device company pioneering MIS sacroiliac (SI) joint treatment. The iFuse Implant System is intended for sacroiliac joint fusion for some causes of SI joint pain. SI joint treatment using the patented triangular design of the iFuse implant has been clinically evaluated more than any other SI joint fusion procedure. More than 100, peer-reviewed publications demonstrate the safety, durable effectiveness, and biomechanical and economic benefits of the iFuse implant (www.si-bone.com/results.) The iFuse implant is the only SI joint fusion device with clinical studies, including two randomized controlled trials1,2, demonstrating that treatment improved pain, patient function, and quality of life.1-6
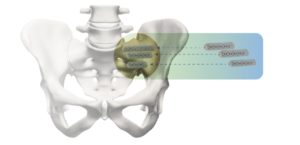
The Fuse Implant System is designed to
provide stabilization and fusion for certain SI
joint disorders.
Indications
The iFuse Implant System® is intended for sacroiliac fusion for conditions including sacroiliac joint dysfunction that is a direct result of sacroiliac joint disruption and degenerative sacroiliitis. This includes conditions whose symptoms began during pregnancy or in the peripartum period and have persisted postpartum for more than 6 months. It is also intended for sacroiliac fusion to augment immobilization and stabilization of the sacroiliac joint in skeletally mature patients undergoing sacropelvic fixation as part of a lumbar or thoracolumbar fusion or for acute, non-acute, and non-traumatic fractures involving the sacroiliac joint. There are potential risks associated with the iFuse Implant System. It may not be appropriate for all patients and all patients may not benefit. For information about the risks, visit www.si-bone.com/risks
References:
1. Polly DW, et al., and the INSITE Study Group. Two-Year Outcomes from a Randomized Controlled Trial of Minimally Invasive Sacroiliac Joint Fusion vs. Non-Surgical Management for Sacroiliac Joint Dysfunction. Int J Spine Surg. 2016;10:Article 28. DOI: 10.14444/3028
2. Dengler J, et al. Randomized Trial of Sacroiliac Joint Fusion vs. Conservative Management for Chronic Low Back Pain Attributed to the Sacroiliac Joint. J Bone Joint Surg Am. 2019;101(5):400-11. DOI: 10.2106/JBJS.18.00022.
3. Duhon B, Bitan F, Lockstadt H, Kovalsky D, Cher D, Hillen T, on behalf of the SIFI Study Group. Triangular Titanium Implants for Minimally Invasive Sacroiliac Joint Fusion: 2-Year Follow-Up from a Prospective Multicenter Trial. Int J Spine Surg. 2016;10:Article 13. DOI: 10.14444/3013
4. Dengler J, et al. on behalf of the INSITE, iMIA and SIFI study groups. Predictors of Outcome in Conservative and Minimally Invasive Surgical Management of Pain Originating from the Sacroiliac Joint – a Pooled Analysis. Spine. 2017;42(21):1664-73. [Epub 2017 Mar 27]. DOI: 10.1097/BRS.0000000000002169
5. Whang PG, et al. Long-Term Prospective Clinical and Radiographic Outcomes After Minimally Invasive Lateral Transiliac Sacroiliac Joint Fusion Using Triangular Titanium Implants. Med Devices (Auckl). 2019;12:411-422. DOI: 10.2147/MDER.S219862
6. Patel V, et al. Prospective Trial of Sacroiliac Joint Fusion Using 3D-Printed Triangular Titanium Implants: 24-Month Follow-Up. Med Devices (Auckl). 2021;14:211-216. DOI: 10.2147/MDER.S314828