WHAT IS A SELECTIVE NERVE ROOT BLOCK?
A selective nerve root block (SNRB) is a test performed to determine if a specific spinal nerve is the source of your arm or leg or radiating chest pain. Often patients with spine issues have multilevel MRI abnormalities often close together. If we treat your problem with conservative care and it fails to respond, then surgery for your radiating pain may be an option. However, due to the above issue identifying which abnormality on the MRI is the cause of the actual radiating pain can be a challenge. In most cases pain that radiates in a radicular fashion as above is caused by just one nerve root regardless of the number of abnormalities on the MRI. Therefore, we are trying, like an electrician would do in your house to find the short circuit, to isolate the responsible nerve that is the source of the pain.
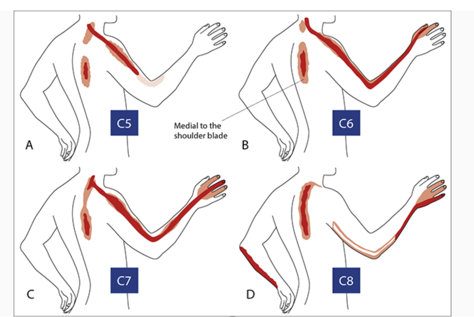
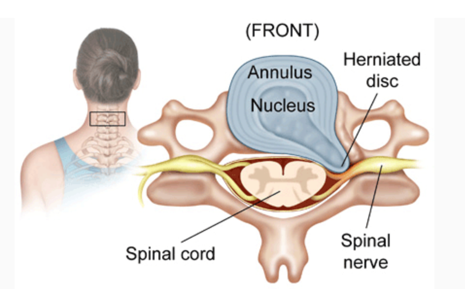
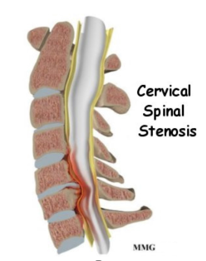
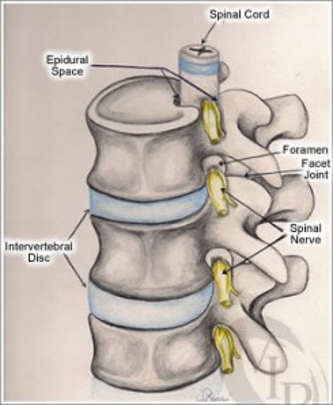
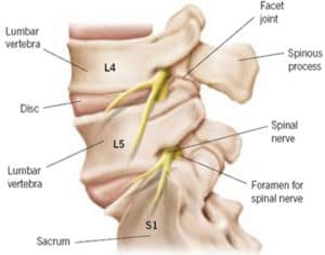
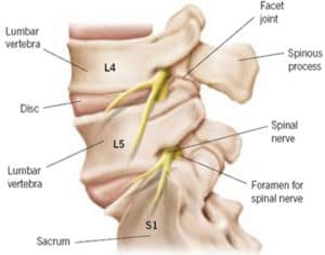
A SNRB is performed to diagnose the specific nerve root of origin of your cervical (neck), thoracic (mid back) or lumbar (low back) radiculopathy (pain in the distribution of a particular nerve root off the spine due to compression, irritation and/or inflammation of a nerve root). A selective nerve root block is an injection of a local anesthetic that lasts hours to a few days very close to a specific nerve root. Along the spine, there are several exit “holes” or “foramina” through which nerve roots emerge. If these foramina are partially closed due to either bony overgrowth from degenerative changes, bulging disks, misalignment of vertebrae, etc., the nerve root can also be pinched. This typically causes a shooting or radiating pain along that nerve root. In a selective nerve root block, a small needle is placed in the foramen alongside the nerve root, and the medication is injected. The goal of a diagnostic injection is twofold. 1. We want to see if the needle adjacent to the nerve creates radiating pain that closely replicates your typical radiating pain for which you are seeking relief. 2. To see if, while the nerve that we injected adjacent to is “asleep” or effectively blocked by the local anesthetic, your normal radiating pain is gone or improved during any period of time while the block is effective. Your feedback helps to identify the cause of radiating pain.
WHY IS IT DONE?
When the nerves in the foramina are irritated or pinched, the resulting inflammation can cause pain, numbness, or tingling. If the local anesthetic is acting on the correct nerve that is causing the pain, then the temporary resolution of pain will provide diagnostic information to your doctor.
HOW LONG DOES IT TAKE TO DO?
The actual injection takes only a few minutes. Please allow about an hour for the procedure; this will include talking to your doctor before the procedure, signing the informed consent, positioning in the room, and observation by the recovery room nurse afterwards.
WHAT MEDICINES ARE INJECTED?
The injection consists of local anesthetic that can last for a few hours to days (e.g., bupivacaine).
WILL IT HURT?
All of our procedures begin by injecting a small amount of local anesthetic through a very small needle. It feels like a little pinch and then a slight burning as the local anesthetic starts numbing the skin. After the skin is numb, the procedure needle feels like a bit of pressure at the injection site. The actual placement of the needle is not painful. However, keep in mind the nerve root is pinched and irritated. If the needle tip brushes against the nerve during placement, you may feel a “zing” down the nerve root, similar to striking your “funny bone”. During the injection of the local anesthetic, there may be a temporary shooting pain along the nerve root’s normal distribution until the local anesthetic sets in, usually in about 15 seconds. These sensations are normal and if they are very similar or identical to the pain that you normally experience then this information is very helpful in confirming the diagnosis of the “pain generator” in your case. It is very important that you let the doctor know doing the injection if you feel the typical shooting pain or not as the needle is nearing your nerve! If the radiating pain you feel during the procedure is not in the normal distribution that you feel this is helpful information as well. If you do not feel any radiating pain, then the needle may not have gotten close enough to the nerve. The medicine could still reach the nerve through diffusion so the block may still give diagnostic information, but we prefer to get the needle as close to a nerve as possible without injuring the nerve.
HOW IS IT DONE?
It is typically done with you lying on your stomach for thoracic or lumbar and on your back for cervical blocks. Your vital signs will be monitored. In addition to your doctor and the x-ray technician, there will be a nurse in the room at all times if you have any questions or discomfort during the procedure. The skin on the back or neck is cleansed with antiseptic solution, and then the procedure is performed.
WHAT SHOULD I EXPECT AFTER THE INJECTION?
Immediately after the injection, you may feel your legs or arms, along that specific nerve root, becoming heavy, numb or weak. You may notice that your pain may be gone or considerably less. This is due to the effect of the local anesthetic. Your pain may return, and you may have some soreness at the injection site for a day or so. It is very important to be careful for several hours afterwards to avoid falling due to weakness if done on the lumbar or thoracic spine or dropping or mishandling things with your hand or arm if done on the cervical spine. This should resolve with the passage of hours but if it persists beyond 8 or so hours please notify our team.
HOW LONG DOES IT LAST?
The immediate effect is from the local anesthetic injected. This wears off at varying time intervals. It may last only 30 minutes, or it may last up to several weeks or months. The length of time that you experience relief is not as important as how much relief you experienced. Please document carefully even hourly for the first day or so. If lucky some even get long term relief of the pain from the nerve block. Of course, that would not only be of diagnostic but therapeutic benefit!
Risks vs Benefits:
Like all procedures or tests there are risks and benefits. The benefit as above is to localize a potential target for surgery when patients have multiple possible causes. The goal here is limiting surgery to the least invasive option possible by treating only the cause of the pain not all the abnormalities on an MRI. The risks include nerve injury, bleeding, post procedure increased pain, allergic reactions, spinal headache, infection and very rarely major neurological complications including the very rare risk of paralysis. Complications are very unlikely and most if they occur can be resolved with treatment. Nevertheless, all procedures and tests have risks.
Conclusion
Selective nerve root blocks are important to help identify the nerve root of origin of your radiating nerve pain. Although the procedure may be uncomfortable, our staff is dedicated to making you as comfortable as possible during the procedure.