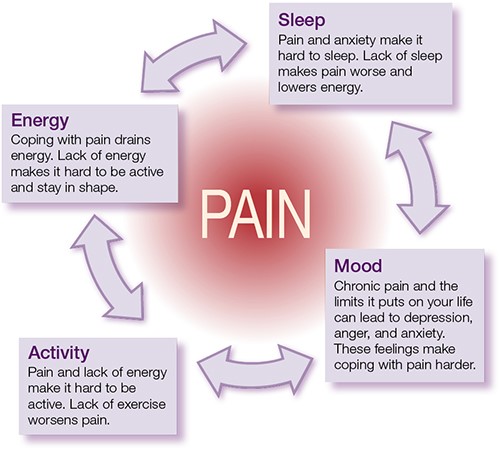
Keep Your Pain Under Control While on the GO
Get comfortable
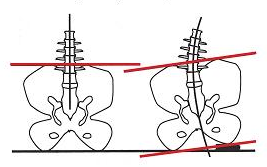
Eliminate any items that could potentially alter your spinal alignment while seated. Remove any objects from your back pocket like a wallet or cell phone. If you are the driver, make sure your seat position is close enough to the steering wheel to avoid reaching.

Get out and move around
Sitting for prolonged periods of time will cause your muscles to tighten and can even lead to spasms. If driving, try to stop every 30-45 minutes for a brief stretch. If you will be on a long flight, make a conscious effort to get up every 30 minutes. Below are a few quick stretches you can do on your short break.

Bring along cold or hot packs
Back pain is often accompanied by inflammation. Ice can help to decrease inflammation and numb any soreness that is a result of prolonged sitting. Some individuals find heat to be more soothing to sore and tight muscles so utilizing heated seats or quick use hot packs can help to ease the ache as well.

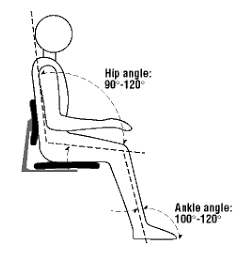
Support your back with your feet
Good support for your back can be strongly influence by foot positioning. Your feet should both be positioned on the floor. Ideally you would like your knees to be at a right ankle in relation to your hips. You may have to modify your seat or utilize a foot rest to achieve optimal positioning.
Have a Diversion
The mind is a powerful thing, so if you are not the driver then use a book or movie to occupy your time. If you are the driver, try music or an audiobook to keep you mind off any pain that may arise from a long trip.
Image credit: https://www.pakwheels.com/forums/t/tips-for-maintaining-pain-free-posture-when-driving-a-car/442532
Image credit: https://wellness-centre.com.au/why-you-should-never-sit-on-your-wallet/
Image credit: https://praktispartners.com.au/latest-news/turn-t-rex-work/